People who have one normal Alpha-1 gene (called M) and one abnormal Alpha-1 gene (S,Z, F, I, other) are often called carriers. Carrier genotypes include MS, MZ, MF, MI, M-Other.
Carriers may be termed “mildly deficient” because this combination of genes leads to a lower Alpha-1 level than expected for most people with two normal genes (MM) but higher than that of someone with severe deficiency caused by two abnormal genes (ZZ, SZ).
Most carriers do not develop Alpha-1 related symptoms; however, recent research has shown that MZ carriers who smoke are at high risk for COPD. MZ carriers also have a small increased risk for liver disease. Carriers should avoid smoking and live a healthy lifestyle.
There are over 20 million Alpha-1 carriers in the US. Being an Alpha-1 carrier is more common than many people know. About 2-3% of North Americans are carriers of the Z mutation (MZ) and about 5% carry the S (MS). Carriers of other mutations such as the F, I, and rare/null mutations are less common and exact rates are not known. A person's individual chance to be a carrier depends on their ethnic background and family history.
The good news is that most carriers never have health problems due to their Alpha-1 mutation. However, research continues to better define select groups of people with higher risk for COPD. It is possible that certain carrier sub-groups with higher risk will be defined in the future. Any person experiencing symptoms or a change in their health should see a healthcare provider for personal evaluation.
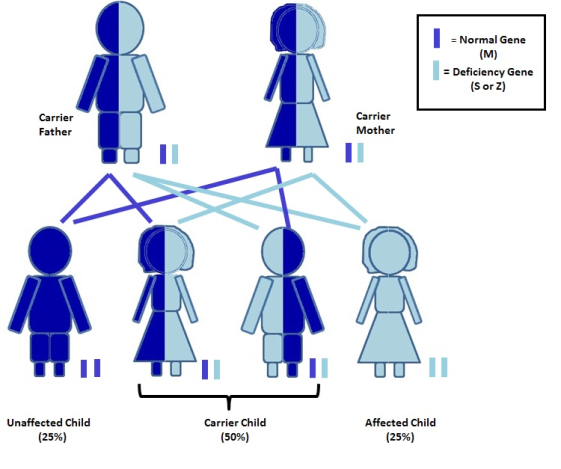
Carriers have a 50% chance of passing on their abnormal Alpha-1 gene to each child, so, any child of a carrier has a 50% chance to be a carrier, too. If two carriers have children together, there is a risk to have a child with severe Alpha-1 antitrypsin deficiency. This happens when the child inherits an abnormal gene from both the mother and the father.